Schlagwort: ‘Encephalitis’
Tick Tock, TBE O’Clock: Your Exam-Ready Guide about Tick-Borne Encephalitis
Disclaimer!
This article and its major media content are produced by students to train science communication as part of a lecture about human infectious pathogens. The article does not represent official advice from the authorities. For authorized information about the disease in question, please refer to the official health authorities in your country or the World Health Organization.
By Franziska Fohn, Gina Auerswald & Jana Egner-Walter
Do you know this moment, where you realize you procrastinated a bit too long and now your virology exam is approaching? Don’t worry! In just a few minutes, here you will learn all the important molecular mechanisms and clinically relevant facts about Tick-borne encephalitis (TBE)—everything you need to answer every question with confidence!
How can TBE replicate and invade the brain?
_
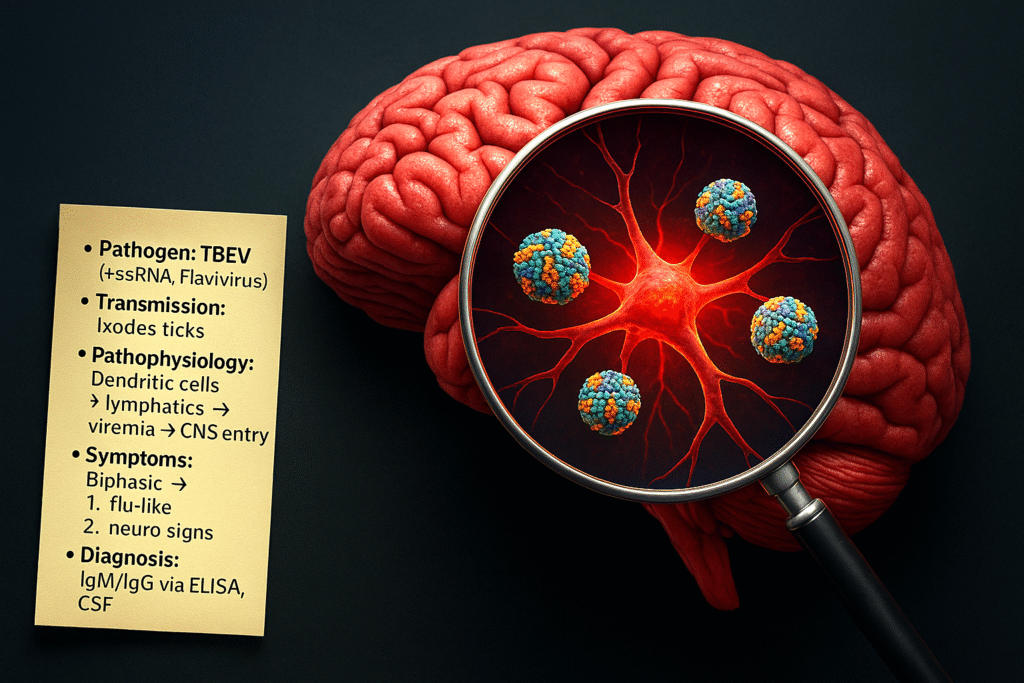
TBE is an infectious disease caused by the TBE-virus (TBEV), a member of the Flaviviridae family. It’s a +ssRNA virus that is transmitted by the saliva during the bite of infected ticks, in Europe mainly Ixodes ricinus. Different properties of tick saliva, such as its antihaemostatic, vasodilatory, and local immunomodulatory activity contribute to the facilitated transmission of TBEV. The virus’s life cycle starts with the uptake of the virion into dendritic skin cells and macrophages via the viral envelope E protein. In these cells, the virus replicates and reaches the lymphatic system. From here on, the TBEV reaches systemic blood circulation, spreading to local lymph nodes and later the spleen, liver and bone marrow. If it breaches the blood-brain barrier (BBB), it reaches the central nervous system (CNS), leading to meningitis or meningoencephalitis. Possible routes by which TBEV may breach the BBB include peripheral nerves; olfactory neurons; transcytosis through vascular endothelial cells of brain capillaries; and diffusion of the virus between capillary endothelial cells. The primary targets of TBEV infection in central nervous system are neurons.
▶ Want a visual explanation of the replication cycle, spread and how neural tissue is affected by TBEV? Check out this 3-minute video from our YouTube Playlist: “Virology with Dr. Vee”*!
How does TBE present clinically and how would you diagnose it?
TBE progresses in a biphasic manner:
- Phase 1 (~ 5 days): After an incubation of about 8 days, the infection starts with flu-like symptoms → fever, fatigue, body aches
- Phase 2: After an asymptomatic week (which may include leukopenia and thrombocytopenia), the virus may attack the CNS → high fever, headache, nausea vomiting, impaired consciousness → meningitis, meningoencephalitis, meningoencephalomyelitis.
During this second phase, typical lab findings include lymphocytic pleocytosis and a higher erythrocyte sedimentation rate (ESR). To confirm TBE diagnosis, two criteria must be met:
-
- Clinical signs of CNS inflammation
- Detection of TBE-specific IgM or IgG in the serum or cerebrospinal fluid (CSF)
Additionally, C-reactive protein (CRP) levels may also be elevated and serve as a marker for disease severity.
▶ Want more information about the clinical experience? Listen to the TBE episode of the podcast “Health Talks”*, in which a patient shares their story, and neurologist Dr. Bennett** provides additional medical insights.
_
How does the TBE vaccine protect from infection?
Since there is no treatment for TBE, prevention through active immunization is crucial. All licensed vaccines against TBEV are based on inactivated whole viruses, containing various TBEV strains. The E-proteins on these inactivated viruses are recognized by dendritic cells through their toll-like receptors (TLRs), leading to the phagocytosis of the particle. The viral proteins are processed and presented on the dendritic cell’s surface via the MHC class II. When migrating to the lymph nodes, they activate CD4+ T-cells, which induce the production of specific antibodies against the TBEV surface markers in plasma cells. In case of a future exposure to TBEV, the antibodies enable a fast recognition of the virus.
Self-test for optimal understanding:
So now that you’ve read all the information, can you answer these (extremely exam-relevant) questions?
- Through which routes may TBEV breach the BBB?
- How does TBEV replicate?
- Which symptoms indicate TBE and how can you confirm the diagnosis?
Don’t forget to follow our Mastodon Account @EasyVirology to stay tuned about upcoming virology study posts!
*fictional YouTube Playlist/Podcast
**fictional character
_
References
- Chiffi G, Grandgirard D, Leib SL, Chrdle A, Růžek D. Tick-borne encephalitis: a comprehensive review of the epidemiology, virology, and clinical picture. Rev Med Virol. 2023; 33(5):e2470. https://doi.org/10.1002/rmv.2470
- Bogovic, P, and Franc S. Tick-Borne Encephalitis: a review of epidemiology, clinical characteristics, and management.“ The Lancet Infectious Diseases, vol. 19, no. 4, 2019, pp. 469–478. https://doi.org/10.1016/S1473-3099(18)30454-1
- Kaiser, R. Clinical manifestations and diagnosis of tick-borne encephalitis. Journal of Neurology, vol. 267, no. 2, 2020, pp. 276–282. https://doi.org/10.1007/s00415-020-09936-w